|
The Indian rural healthcare system, while seeing improvements over time, continues to be very weak as seen from the much lower than recommended levels of workforce availability (including specialists), paucity of hospital beds availability per capita, poor infrastructure and quality of care. Adequate and affordable healthcare is still a long way away. Access to reliable electricity is a critical infrastructure input for the delivery of effective healthcare services. This crucial aspect of public healthcare has somehow escaped wider public discourse. This is evident due to the fact that, in spite of the guidelines from the Indian Public Health Standards (IPHS) regarding uninterrupted power supply, a very high number of rural healthcare centres remain without access to electricity and those with access very likely face serious issues about reliability. Taking advantage of the ever-reducing prices and modularity of battery storage and solar power, this article proposes adoption of battery storage systems to meet the challenge of providing uninterrupted and high quality power supply to rural healthcare centres as well as Sub Divisional and District Hospitals. It also explores providing electricity access through solar+storage to existing and upcoming centres in remote and hilly areas to increase equitable access to healthcare. The article outlines a broad strategy for centralised bulk procurement of battery storage systems/services with adequate government support. This will give a huge fillip to transforming rural healthcare services and should be an integral part of the Ayushman Bharat Health Infrastructure Mission2. |
It is quite self-evident that reliable electricity is paramount for the delivery of effective healthcare services. A recent paper exploring this issue, Reduced health services at under-electrified primary healthcare facilities: Evidence from India by Shastry et. al notes that, ‘One key infrastructure gap is access to reliable electricity, absence of which can significantly affect the quantity and quality of healthcare services being delivered at rural primary health facilities. Their analysis leads them to conclude that, ‘lack of electricity access is associated with a significant and large decrease in the number of deliveries (64 percent), number of in-patients (39 percent), and number of out-patients (38 percent). Lower level of electricity access at primary health centers is disproportionately associated with adverse effects on women’s access to safe and quality healthcare’. Thus, providing electricity with very high reliability is one essential element to the success of healthcare provision and can also contribute to reducing the gender gap.
Taking advantage of the ever-reducing prices of energy storage3 and its modularity, this article discusses the adoption of battery storage units to meet the twin challenge of providing uninterrupted and high quality power supply to healthcare centres as well as providing access (through solar+storage) to existing and new centres in remote and hilly areas to increase equitable access to healthcare. This article is Part 3 of a three-part series to discuss financially viable ideas to improve electricity service delivery for meeting India’s developmental goals in a post-covid world.
1. Status of electricity access in rural healthcare facilities
The Rural Health Statistics 2019-20 makes for sobering reading. While there has been growth in the availability of healthcare services over the years, there is still an extremely long way to go in providing quality healthcare as seen from the various statistics of shortfall in human resources (doctors, specialists, healthcare workers, nurses, technicians, paramedical staff) and infrastructure (electricity, regular water supply, motorable road, telephone, computers etc) prevalent across India.
|
Overview of RURAL HEALTH CARE SYSTEM IN INDIA (Rural Health Statistics 2019-20) The health care infrastructure in rural areas has been developed as a three tier system. As on 31st March, 2020, there are 1,55,404 Sub Centres (SC), 24,918 Primary Health Centres (PHCs) and 5,183 Community Health Centres (CHCs) which are functioning in rural areas of the country. Sub Centre (SC): Most peripheral contact point between Primary Health Care System & Community. Sub Centres are assigned tasks relating to interpersonal communication in order to bring about behavioural change and provide services in different programmes like maternal and child health, family welfare, nutrition, immunization, diarrhoea control and communicable diseases as well as noncommunicable diseases. Primary Health Centre (PHC): A Referral Unit for 6 Sub Centres 4-6 bedded manned with a Medical Officer In-charge and 14 subordinate paramedical staff. PHC is the first contact point between village community and the medical officer. The PHCs were envisaged to provide an integrated curative and preventive health care to the rural population with emphasis on preventive and promotive aspects of health care. The PHCs are established and maintained by the State governments. Community Health Centre (CHC): A 30 bedded Hospital/Referral Unit for 4 PHCs with Specialized services. CHCs are being established and maintained by the State government. CHC is required to be manned by four medical specialists i.e. Surgeon, Physician, Obstetrician/Gynaecologist and Paediatrician supported by 21 paramedical and other staff. It has 30 in-door beds with one OT, X-ray, labour room and laboratory facilities. |
Here, we limit our focus to the electricity component within the ailing healthcare infrastructure. As seen from Table 1, a large number of Sub Centres (28%) presently do not even have access to electricity, with the same number just under 5% for PHCs. Considering the shortfall in healthcare centres and the likelihood that these new facilities, as and when they come up would be located in even more remote rural areas, the electricity access issue is not likely to be resolved immediately. This is also borne out by Figure 1 which shows that significantly more SCs are without electricity access compared to PHCs and the share of SCs without access has also slightly increased over the last decade. Further, these centres without access are concentrated in few states, namely Uttar Pradesh, Bihar, Rajasthan as seen in Table 2.
A number of services offered by these centres including operatives (caesarean section, medical termination of pregnancy, sterilization, minor surgeries) in some PHCs and all levels above PHC, vaccine storage facilities, normal deliveries in PHCs and some sub-centers etc. depend critically on reliable power supply. SCs are mainly entrusted with services catering to women and children (delivery, vaccination). Thus just the expanded health care availability (increasing number of PHCs and SCs) may not necessarily translate to better health outcomes if there is no access to reliable power supply.
The Rural Health Statistics 2018-19 points to another data-point, namely the number of rural Health and Wellness Centres (upgraded SCs) which have electricity along with power back up. Of the 7,821 HWCs in rural India, only 3,496 (45%) have an electricity back-up facility.
Figure 1. Proportion of PHCs and SCs Without Electricity Supply
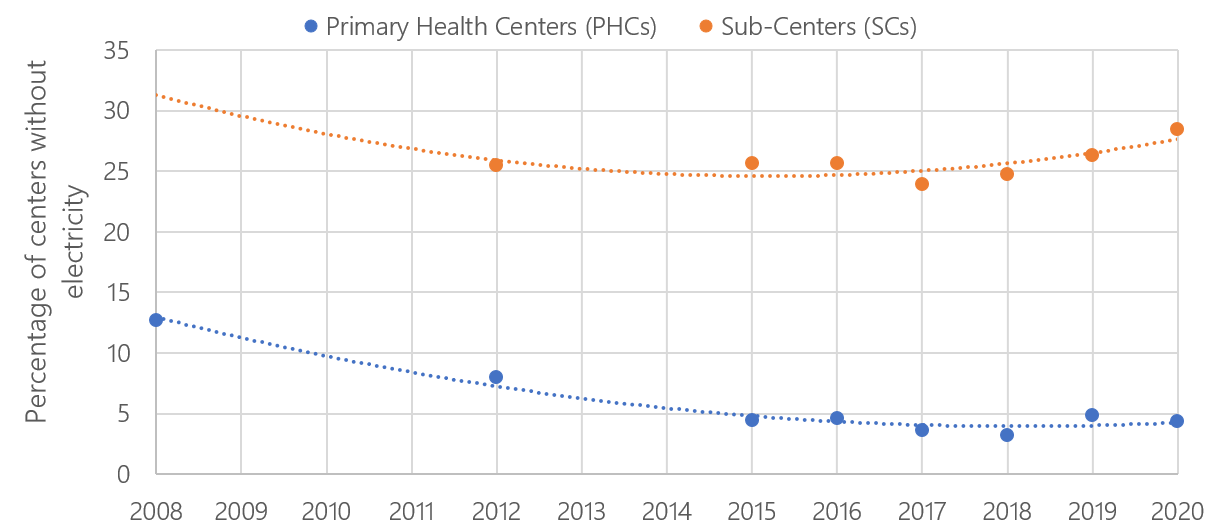
Source: Shastry V, Rai V (2021) Reduced health services at under-electrified primary healthcare facilities: Evidence from India. PLoS ONE 16(6): e0252705. https://doi.org/10.1371/journal.pone.0252705; Appendix.
Table 1. Existing rural healthcare centres, shortfall and centres without access to electricity as of March, 2020
| Status | Sub Centres | Primary Health Centres (PHCs) | Community Health Centres (CHCs) |
| Functioning | 1,55,404 | 24,918 | 5,183 |
| Required | 1,91,461 | 31,337 | 7,820 |
| Shortfall | 36,057 | 6,419 | 2,637 |
| Shortfall (%) | 23% | 26% | 51% |
| Without electric supply | 44,081 | 1,076 | |
| Without electric supply (%) | 28.4% | 4.3% |
Source: Prayas (Energy Group) compilation from Rural Health Statistics, 2019-20
Table 2. States with highest share of PHCs and SCs in rural areas without electric supply as of March, 2020
| SUB CENTRES | PRIMARY HEALTH CENTRES | ||||
| State | Number of SCs without electric supply | % of total SCs without electric supply | State | Number of PHCs without electric supply | % of total PHCs without electric supply |
| Uttar Pradesh | 15,614 | 35% | Bihar | 282 | 26% |
| Bihar | 5,005 | 11% | Jammu and Kashmir | 172 | 16% |
| Rajasthan | 4,695 | 11% | Uttar Pradesh | 133 | 12% |
| Karnataka | 2,777 | 6% | Rajasthan | 77 | 7% |
| Odisha | 2,768 | 6% | Jharkhand | 65 | 6% |
| All India | 44,081 | 100% | All India | 1076 | 100% |
Source: Prayas (Energy Group) compilation from Rural Health Statistics, 2019-20
2. Guidelines for electricity infrastructure for healthcare facilities
The Indian Public Health Standards (IPHS) lays down guidelines for District/Sub-District/Sub-Divisional Hospitals as well as for Sub-Centres, PHCs and Community Centres4. Guidelines related to electricity are noted in the table 3 below and clearly show the critical need for reliable electricity supply. Further, as per the Clinical Establishment Act Standards for Hospital (LEVEL 1A &1B hospitals) ‘shall have 24 hr supply of electricity, either through direct supply or from other sources’.
Table 3. IPHS guidelines related to electricity
| Type of Health Care Centre/Hospital | Excerpts from the guidelines related to electricity |
| Sub-Centres | Electricity: Wherever facility exists, uninterrupted power supply has to be ensured for which inverter facility/solar power facility is to be provided. Generator facility is made available at Type B Sub-centres. (pp. 17) |
| PHCs | The area chosen should have facilities for electricity… (pp. 12); Requirements for a fully equipped and operational labour room: Electricity supply with back-up facility (generator with POL) (pp. 24) |
| Community Centres | The area chosen should have facilities for electricity… (pp. 11); Blood storage facilities- Electricity: 24 hours supply is essential. Provision of back-up generator is required. (pp. 65, Annexure 11) |
| Sub-District/Sub-Divisional Hospitals (31 to 100 Bedded) | Sub Station and Generation: Electric sub station and standby generator to cater for the full load of the hospital should be provided. (pp. 24) |
| District Hospitals (101 to 500 Bedded) | Electric Engineering Sub Station and Generation Electrical load requirement per bed = 3 KW to 5 KW. Electric sub station and standby generator room should be provided. (pp. 35) |
Source: IPHS, compiled by Prayas (Energy Group)
3. Lack of reliable electricity supply in rural areas
While the data in section 1 gives an indication of rural centres with access to electricity, anyone familiar with rural India would ascertain that simply having access is not necessarily equal to having reliable, uninterrupted supply with high level of quality. Public data on quality of supply is limited and ad-hoc in nature. We at Prayas (Energy Group) have been running the Electricity Supply Monitoring Initiative (ESMI) which provides evidence based feedback of electricity supply quality5 at residential locations across India. We find that consumers often face poor quality supply in the form of frequent interruptions, load shedding / blackouts, and low voltage levels. Hours of supply and reliability in rural health centres is likely to be very similar to these residential locations. Beyond mere hours of supply, the time of day when electricity is interrupted is also crucial for health care delivery. Equally crucial is the duration of the power cuts, since longer duration cuts can break the cold chain and affect storage of vaccines amongst other things.
Figure 2 shows the hours of supply for rural locations in few states in 2019. For no location do we see 24X7 reliable supply, a basic requisite for healthcare facilities. The range of daily hours of supply is quite significant and varies across locations and months. Another survey of 3000 households in Maharashtra and Uttar Pradesh conducted by us, further corroborates this6. Finally, our eMARC initiative, which collects minute-wise data on electricity consumption using smart meters from a sample of households and appliances bring out this issue more starkly. Data for 115 households from January 2018 to June 2020 from Pune City and semi-urban and rural households from the districts of Pune, Aurangabad, Kanpur Rural, and Gonda shows ‘significant variation in the quality of electricity supply observed particularly in the semi-urban and rural areas of all the four districts’. The data also shows the poor quality of supply as evinced from the voltage data which show both high and low levels which in turn can damage appliances, pose safety risks and prompt investments in protective equipment such as voltage stabilizers and surge protectors. Poor quality of electricity supply results in restricted use of appliances as well as increased costs of running the appliances.
Thus while hours of supply have improved in recent years, there is still a long way to go to reach reliable 24X7 supply; and the importance of this in the context of life saving appliances cannot be overstated.
Figure 2. Hours of electricity supply in some rural areas in 2019
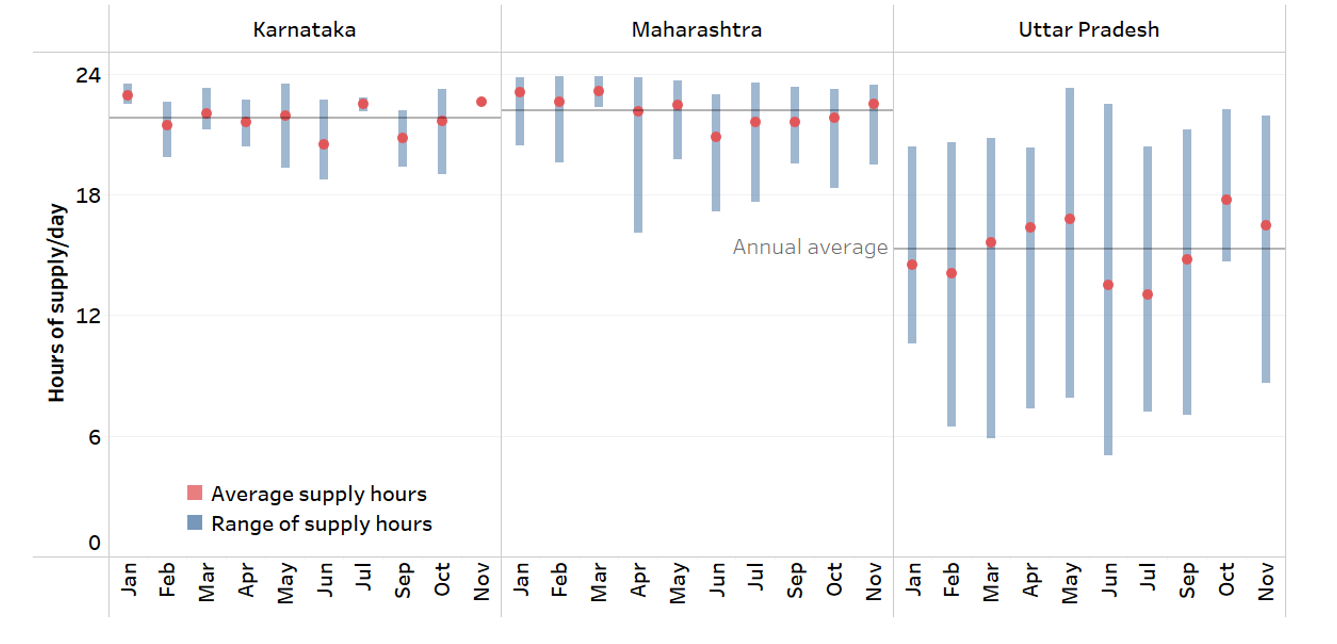
Source: www.watchyourpower.org; Electricity supply monitoring initiative from Prayas (Energy Group). Data for 57 locations. Data for Aug and Dec not shown due to low availability. Range is from the minimum and maximum average daily hours of supply at some locations in that state.
4. Shifting from diesel gensets to battery storage for improving reliability and providing access
The health care sector has a high share amongst users of diesel gensets for back-up power. This is to be expected given the poor quality of supply and the need for reliable 24X7 power in healthcare. The ever increasing costs of diesel (Rs 90/litre in Delhi as of Oct, 2021) coupled with diesel’s contribution to worsening air quality makes for a good case for considering alternatives. The Ministry of Power (MoP) has initiated some steps in this regard.
As per the Draft Electricity (Rights of Consumers) Amendment Rules, 2021, the MoP has proposed a new rule 10(3) which notes that ‘In view of the increasing pollution level particularly in the metros and the large cities, Distribution Licensee shall ensure 24x7 uninterrupted power supply to all the consumers, so that there is no requirement of running the Diesel Generating sets.’ It further notes that, ‘Consumers, who are using the Diesel Generating sets as essential back up power, shall endeavor to shift to cleaner technology such as RE with battery storage etc in five years from the date of the publication of this amendment or as per the timelines given by the State Commission for such replacement based on the reliability of supply by the distribution company in that city.’ (emphasis own)
While the focus of this rule seems to be on urban areas, there is no reason why this must not be implemented across the country. Battery storage pack prices, especially those based on Li-ion chemistries have fallen dramatically in the last decade, from $1,100/kWh in 2010 to $137/kWh in 2020, a drop of 89% in real terms. There are projections for these to further drop by over 50% in the coming decade7. Apart from their increasing cost advantage, they are extremely modular in deployment and have very low gestation periods, and land/space requirements. They have extremely quick response times (on the order of milli-seconds) and can thus be a valuable contributor to providing reliable, uninterrupted and quality 24X7 supply, especially in critical social and economic applications such as healthcare. The importance of battery storage is already outlined in the ‘National Mission on Transformative Mobility and Battery Storage’ approved by the Cabinet in March, 2019.8
5. Proposed scheme to improve reliability in existing healthcare centres and provide access in remote areas.
We propose that the GoI come up with a new national program on providing reliable and quality 24X7 supply to all healthcare services (especially in rural areas with more immediate needs) through the deployment of battery energy storage systems (BESS). Agencies such as EESL or SECI would aggregate demand from various rural healthcare centres for a district/state and facilitate bulk procurement, deployment along with operation and maintenance of these standardised systems. Large-scale procurement would further reduce costs, even as the existing counterfactual for back-up power through diesel gensets is already very costly. MNRE or MOHFW would provide graded declining incentives/subsidies (say 75%/50%/25%) over the years linked to specific milestones, thereby encouraging early adoption by states/DISCOMs. Pre-defined sunset period for incentives/subsidies (say for 5 years) linked to market prices is necessary to avoid any hindrance for long term industry development9. Appropriately sized BESS could also bring in much needed resiliency in the power supply situation for this critical public service.
These investments/projects should be set up as service contracts by EESL/SECI and the full costs repaid/amortised over ten years. This would make the yearly payments for new BESS deployment even more manageable and put the onus of performance and O&M on the developer. One could structure payments as a two-part tariff to ensure project quality and developer’s interest in the long run. Alternatively, GoI could bear part of the costs as a grant and the balance could be socialised to all consumers as part of the DISCOM’s ARR. DISCOM could keep track of the value of energy storage system by ensuring separate monitoring, accounting and possible commercial settlement.
Different actions are needed in order to overcome the lack of electricity access in remote areas and unreliability in existing centres, but there are overlaps. To begin with, in phase 1, the focus could be limited to rural areas where the need is the highest. As seen in Table 1, there are over 45,000 Sub Centres and PHCs without access to electricity and over 42,000 are yet to be built.
Solar + Storage for providing electricity access in remote/rural healthcare centres
Solar + battery storage units should be considered for centres (existing and yet to be built), especially in extremely hilly and remote regions without access. Sizing of BESS and solar+storage would depend on the size of the centre and the number of patients availing services. A few standardised sizes could be allowed to be chosen from depending on the size of the centre.
Battery storage systems for improving supply reliability in centres with electricity access
For existing centres where reliability is low or of paramount importance, replacing diesel back-up with battery storage should be the focus. Of the existing 1.35 lakh PHCs and SCs with electric supply, if one provides them with an average BESS of 50 kWh size, this will imply a total procurement of 6.7 GWh and will need a total investment of Rs 12,670 crore (assuming an average cost of $ 250/kWh and exchange rate of Rs 75/USD). Considering an 8% rate of interest and repayment over a 10-year period, this would translate to an annual payment of Rs 1,845 crore. To put this in context, the Ministry of Health and Family Welfare received an allocation of Rs 67,112 crore in 2020-2110.
While the lack of reliable electricity and access is especially striking in PHCs and SCs, it still remains an issue at higher tiers of public healthcare as well. Thus, this scheme could be taken further than PHCs and SCs. As of March 2020, India has 1,193 Sub Divisional Hospitals (SDH) and 810 District Hospitals. Surveys benchmarking electricity consumption in govt. hospitals note an annual consumption of 0.5-1.8 GWh/year depending on the size, no. of beds etc. (Source: BEE). This translates to an average daily use of 1.5-5 MWh. Deploying standardized electric storage projects/services in such hospitals for improving the reliability/resiliency of supply and reducing the use cost, diesel power generation would be a great example of combining a critical social need with electric storage deployment at scale. A 0.5 MWh battery at each of the SDH and DHs would translate to a total bulk procurement of ~1 GWh. Assuming an average cost of $ 250/kWh and exchange rate of Rs 75/USD, this would roughly translate to an overall cost of Rs 1875 crore. Assuming the same financing options, it translates to an annual payment of Rs 273 crore.
Table 4. Indicative resource requirements for improving reliability through battery storage
| PHCs and SCs | Sub Divisional Hospitals and District Hospitals | |
| Number | 1,35,165 | 2,003 |
| Average BESS size (kWh) | 50 | 500 |
| Total BESS procurement (GWh) | 6.8 | 1 |
| Total investment ( Rs crore) | 12,672 | 1,878 |
| Annual payments (Rs crore) | 1,845 | 273 |
Assumptions: Avg BESS cost: $ 250/kWh; Exchange rate: Rs 75/USD; interest rate: 8%; repayment: 10 years.
6. Concluding thoughts
As noted in Shastry V, Rai V (2021), there is a ‘strong case for rural health system planners and government health departments to pay much more attention to understanding and integrating reliable energy access as an enabler of more equitable access to primary healthcare’. Further, ‘given that the HWCs will be more decentralized and spread out than PHCs, it is imperative that reliable electricity access be considered an integral part of the strategy for developing HWCs’.
Considering the poor situation of electricity access and quality of supply in rural India, it is imperative to overcome this problem, especially for a critical need such as healthcare. BESS can supplement the efforts in improving supply reliability and resiliency and considering the ever-reducing prices, can be rapidly and cost-effectively deployed at scale. This can prove to be a critical input to transforming rural healthcare services.
Endnotes
1. This article is part of an ongoing series called Power Perspectives which provides brief commentaries and analyses of important developments in the Indian power sector, in various states and at the national level. Comments and suggestions on the series are welcome and can be addressed to
What is Ayushman Bharat Health Infrastructure Mission?
In a bid to increase accessibility, the Ayushman Bharat Health Infrastructure Mission, an addition to the National Health Mission, will provide support to 17,788 rural Health and Wellness Centres in 10 ‘high focus’ states and establish 11,024 urban Health and Wellness Centres across the country. According to a press release by the Prime Minister’s Office, the mission’s objective is to “fill critical gaps in public health infrastructure, especially in critical care facilities and primary care in both the urban and rural areas.”
5. This is done through IoT based Electricity Supply Monitors (ESM) which track supply interruptions and voltage levels at consumer locations. The ESM is a plug-in device that integrates a voltage recorder and a data-logger and can be easily installed at any remote location. The ESM records voltage by the minute at its location and sends the data to a central server using GPRS.
9. Like the case of the wind power sector being overly dependent on the Accelerated Depreciation tax benefit in the past.